Category
Your Kidney Disease Questions Answered
Did you know that March is National Kidney Month? These vital organs perform some of the most important, life-sustaining functions in the body—but over time, they can become damaged, with little to no warning.
Today, more than 30 million people have chronic kidney disease. Chances are you know someone who has it—or who is at high risk. But what exactly is kidney disease and how can you prevent it? We had a chance to speak with Jerry McCauley, MD, MPH, director of Jefferson’s Division of Nephrology, to learn more about kidney disease symptoms, treatment, and prevention.
Q: What is kidney disease?
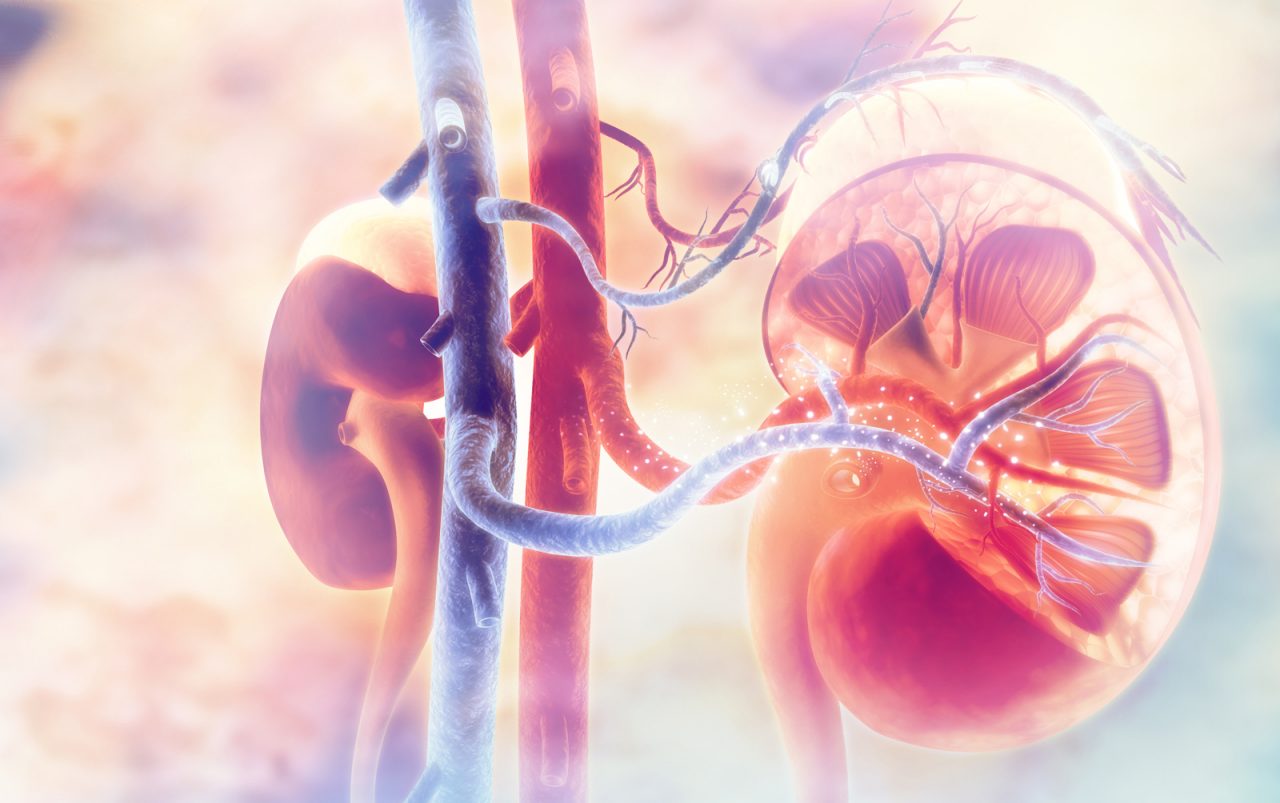
A: The kidneys are vital organs that remove waste products and toxins from the body. The kidneys also maintain proper water and electrolyte balance and produce hormones for hemoglobin synthesis and bone health. Damage to the kidneys can result in
- Salt and water retention leading to swelling in legs
- Hypertension or high blood pressure
- Anemia
- Bone pain and fractures
- The buildup of toxins in the body
- Increased risk of cardiovascular disease such as heart failure and heart attack.
Kidney disease can happen acutely in states such as dehydration and infection, or with exposure to nephrotoxic drugs. Chronic kidney disease (CKD) is a progressive condition that develops gradually over months to years and can result in irreversible damage to the kidneys.
Q: What are the symptoms of chronic kidney disease?
A: CKD can be a silent disease initially. Symptoms are initially vague and become more pronounced in advanced stages of the disease. These include
- Nausea
- Fatigue
- Decreased urination
- Waking up multiple times during the night to urinate
- Abnormal metallic taste in mouth
- Itching
- Decreased appetite and weight loss
- Swelling all over body
- Difficulty breathing
- Uncontrolled high blood pressure
Q: When should you see a doctor?
A: If you have the following risk factors and/or conditions, you should be regularly assessed by your primary care physician:
- Risk factors for kidney disease such as high blood pressure, Type 1 diabetes, or long-standing Type 2 diabetes
- A family history of kidney disease
- Recurrent urine infections
- Lupus
- Kidney stones
Any significant abnormality should warrant a nephrology consultation.
Q: When does a doctor decide to test for kidney disease?
A: If you have any of the risk factors for kidney disease, it becomes important to evaluate your baseline kidney function and monitor it vigilantly.
Q: What kinds of tests are involved?
A: Initial tests include blood tests, urine analysis, and CT scans that are cost effective and performed by primary care physicians.
Q: What are some common causes of kidney disease?
A: The most common causes of kidney disease are diabetes and hypertension, which account for more than two-thirds of patients with end-stage kidney disease that requires kidney dialysis and transplantation.
Q: How does diabetes impact kidney disease?
A: Diabetes remains the leading cause of chronic kidney disease and end-stage renal disease in this country. The presence of kidney disease in diabetics puts them at increased risk of poor quality of life and death due to cardiac disease. Therefore, the detection and management of kidney disease is critical, especially for people with diabetes.
Q: Is there a cure?
A: Kidneys have a high capacity to heal in case of acute injury. However, multiple episodes may lead to scarring and chronic impairment. Prevention is the prime focus of disease management, since not all forms of kidney disease are curable. Dialysis can substitute for failed kidneys for life. The kidney is the most transplantable solid organ in the U.S. Every dialysis patient—and those with advanced kidney disease not yet on dialysis—are eligible for transplant evaluation.
Q: Is a person with kidney disease limited when it comes to activities like exercise, eating certain foods, etc.?
A: Lifestyle modifications to incorporate dietary changes, exercise, abstinence from smoking, and maintaining a healthy weight are pivotal for patients at all stages of kidney disease. At later stage kidney disease, your doctor might advise you to curtail foods rich in potassium based on your labs. Salt restriction in diet is essential for blood pressure control and for antihypertensive medications to be effective.
Q: What sets Jefferson apart from other hospitals when treating kidney disease?
A: Jefferson provides integrated care of patients with kidney disease that involves specialists who have long-standing experience in treating diabetic kidney disease, glomerulonephritis, hypertension, and nephrolithiasis. Our physicians focus on treating health in totality with a focus on cholesterol management, gout, hypertension, and BMI in addition to the kidney disease. We use every opportunity to educate our patients and to provide resources available in the community such as Kidney Smart classes for patients with Stage 3 CKD and beyond. And because we have a multidisciplinary team of surgeons, urologists, and hepatologists, we are able to obtain expert consultations within the same institute for our patients.